Several medical professionals that I follow on Twitter have excitedly announced the arrival of this joint article: A multinational Delphi consensus to end the COVID-19 public health threat, in Nature. The panel of 386 experts from 112 countries developed a set of 41 consensus statement and 57 recommendations, which have been further endorsed by 184 organizations globally. Steffen has a super short version:
So much of this has already been said, but the fact that there is consensus from so many gives it just that much more weight: We need to communicate effectively, strengthen health systems, emphasize vaccination but not exclusively so, promote preventative behaviours, expand treatments, and eliminate inequities. Their recommendations are to be implemented in the short term (months, not years) "to end COVID-19 as a public health threat. . . . Failure to use these approaches risks not only prolonging COVID-19 as a public health threat, but also further diversion of resources from efforts to achieve other extant public health goals." Below are some of the important bits.
Three of the highest-ranked recommendations call for the adoption of whole-of-society approaches, while maintaining proven prevention measures using a vaccines-plus approach [vax, mask, ventilate/filtrate]. . . . advise governments and other stakeholders to improve communication, rebuild public trust and engage communities in the management of pandemic responses. . . .
Pandemic fatigue threatens to undercut our vigilance and the effectiveness of our responses to ongoing and new pandemic-related challenges. . . . Highly transmissible variants continue to spread globally. . . . Reinfection risks are not fully understood. . . . Long COVID has emerged as a serious chronic condition that represents a considerable burden of disease and still lacks adequate understanding and appropriate preventive or curative solutions. In addition to its direct health consequences, COVID-19 has disrupted economic activity, social interactions and political processes, affected civil liberties and interrupted education at all levels. Although many government and individuals no longer have the same level of concern as earlier in the pandemic, many public health leaders, including members of this panel, continue to regard COVID-19 as a persistent and dangerous health threat. . . .
There is information fatigue and waning compliance with those public health and social measures that remain in place. . . . Meanwhile, during periods of high community transmission, needs for services continue to exceed the capacity of many health systems, which also are challenged by ongoing risks to the health of their workers. Furthermore, long-standing social inequities have caused some populations to experience greater risk of COVID-19 infection, severe disease and death.
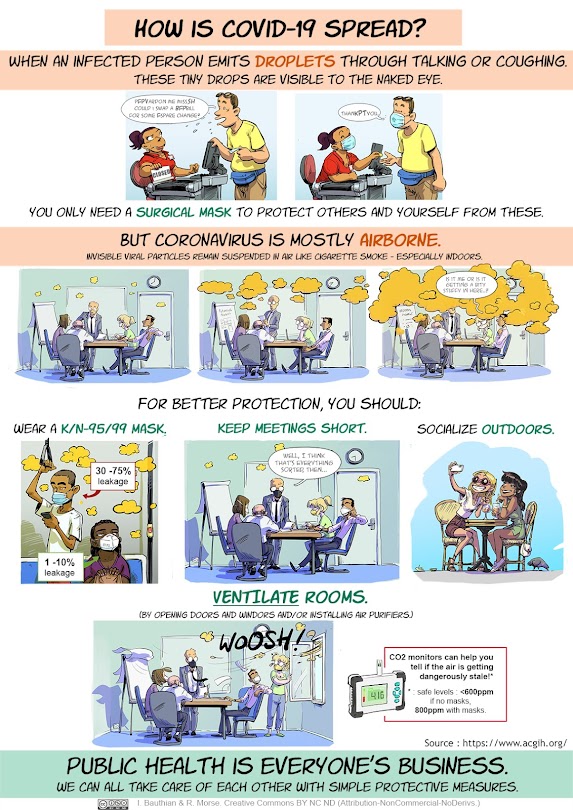
On that front, a friend and I put together this infographic (front and back) - share widely!
From Table 3:
SARS-CoV-2 is an airborne virus that presents the highest risk of transmission in indoor areas with poor ventilation. . . . Relying on individual, voluntary compliance with transmission prevention measures is insufficient to end COVID-19 as a public health threat. . . . Infection rates tend to increase when government discontinue social measures, including non-pharmaceutical interventions, regardless of the level of vaccination. Wide use of high-filtration and well-fitting facemasks (for example, N95...) is important to reduce transmission, particularly in high-risk settings. Most countries have not adequately protected children throughout the pandemic. . . .
Prioritizing the treatment of severe COVID-19 over the prevention of SARS-CoV-2 transmission risks increasing infections, long COVID and the overall burden of disease. . . . The decision by most high-income countries to protect intellectual property rights for COVID-19 vaccines and treatments has contributed to limited options available to low- and middle-income countries. . . . The incorporation of research paradigms from diverse disciplines has greater potential to end COVID-19 as a public health threat than reliance on a single research paradigm.
From Table 2:
Public health authorities contribute to the dissemination of false information when their communications do not reflect current scientific understanding that transmission of SARS-CoV-2 is primarily airborne.
This exchanged just happened today: my local Public Health Unit got pounced on a bit for putting hand-washing first and not even mentioning mask use, and then they withdrew the tweet:
Governments have inconsistently counteracted false information in the context of the COVID-19 pandemic. Sources of false information undermine the social cohesion needed for an effective public health response. . . . When the risk of harm to others is sufficiently severe, governments may determine that the right of all individuals to good health overrides the autonomy of any one individual to choose not to be vaccinated. . . . Vaccination alone is insufficient to end the COVID-19 pandemic. Governments have inconsistently counteracted false information in the context of the COVID-19 pandemic.
From Table 4
Community leaders, scientific experts and public health authorities should collaborate to develop public health messages that build and enhance individual and community trust and use the preferred means of access and communication for different populations. . . . Public health professionals and authorities should combat false information proactively based on clear, direct, culturally responsive messaging that is free of unnecessary scientific jargon. . . . Healthcare organizations should support their workers' physical, mental and social well-being.
From Table 5
Public health policy should take better account of the potential long-term impact of the unchecked spread of COVID-19, given ongoing uncertainties about the prevalence, severity and duration of post-COVID-19 morbidity (long COVID). To reduce the burden on hospitals, primary care should be strengthened to include testing, contact tracing, the monitoring of mild symptoms and vaccination.
From Table 6
National and international travel restrictions should be based on current scientific knowledge and prevailing transmission rates of all variants that take into account relevant, health-based factors (for example, traveller's vaccination status, proof of recent recuperation from COVID-19 or a negative result of an antigen or PCR test). All countries should adopt a vaccines-plus approach that includes a combination of COVID-19 vaccination, prevention measures, treatment and financial incentives. Prevention of SARS-CoV-2 transmission in the workplace, educational institutions and centres of commerce should remain a high priority, reflected in public health guidance and supported through multiple social measures and structural interventions (for example, remove work/schooling policies, ventilation, air filtration, facemask wearing).
They end with this: None of us is safe until everyone is safe.
Here's another great graphic on spread:





No comments:
Post a Comment