Another NEW study shows, yet again, that SARS-CoV-2 is harmful to kids. Who knew?!?
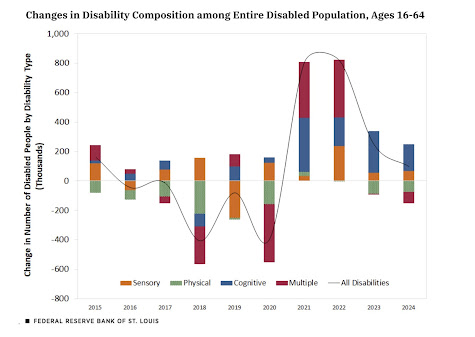
This was a three-year study that followed 1319 children after a first infection. Almost all of the kids had a mild (89%) or asymptomatic (9%) initial infection. Almost 80% were unvaccinated. At 3 months post acute infection, almost a quarter of the kids had Long Covid. From 1-2 years 7 to 8% continued to have Long Covid. Some of the kids infected at the very beginning of the study, still had Long Covid at the 3 year mark. We're generally being told the chance of Long Covid is somewhere between 7 and 10% (the CDC pegged it at 20% earlier), but that misses the reality that many more kids are sick for months before recovering.
Important to note: only 67% had a fever as part of their acute infection, yet that is STILL the only symptom we look for to determine if kids should go to school. Having a runny nose was the next most common symptom, but fewer than half had that (46%). Covid shows up in a multitude of symptoms. The current variant goes for the GI system, so diarrhea is an important sign.
Who gets Long Covid? They found that teenagers (kids over 12) are significantly more in danger. And girls tend to get it slightly more than boys. They indicate that vaccination was protective, but I'm confused by their data, which make it seem like it isn't at all: They compare all patients to unvaccinated, and the unvaccinated numbers with Long Covid are lower across the board, but I must be misunderstanding something there.
At any rate, Covid really, really damages kids. A quarter will lose out on at least three months of school and life at a very pivotal age, and 7-8% will lose years of their lives, possibly the rest of their lives to a chronic illness. I'm not sure how many more studies we need before schools will overtly and regularly start at least encouraging masks in class and before hospitals will mandate them everywhere. How bad does it have to get?? We know that kids (and adults) with a mild infection can go on to develop organ failure. Our only tool right now is prevention with good quality masks while we wait for the clean air revolution to kick into gear.
Yesterday I posted this article, explaining that it's up to parents to take the lead, but I didn't summarize the tragic story it contained: A 16-year-old girl, Cara, who always masked at school to protect her mom dealing with chemo, was convinced to finally take it off. She got Covid, and brought it home, and her mother died, and now she has to cope with the guilt of that on top of her grief. The article says she was bullied as the only person masking in the school, but then explains that she stopped when she heard a child psychotherapist on the radio say that girls wear them to hide their acne. That was the last straw for her.
From the article,
"In 2022, over six times as many children died from Covid than from flu in the US. The UN Convention on the Rights of a Child requires states to 'recognise the right of the child to the enjoyment of the highest attainable standard of health' and to fully implement this right. Children's rights to education include a safe environment not harmful to their health. Cara and her parents fought for these rights. They were denied, with devastating consequences."
I can do absolutely everything I enjoy publicly with a mask on except to eat in a restaurant. So I order in for special occasions. Once you get used to it, masks don't hamper the pleasure of the event, AND you don't get or inadvertently spread a disabling, fatal virus to anyone!! It's win/win!! I understand that a tiny percentage of people actually can't wear a mask, but I cannot accept the argument that mask are uncomfortable or feel suffocating when the alternative to wearing a mask is children and their parents getting sick like this or dying.
Grow. The fuck. Up.